How do mental health issues impact the likelihood of food security? This question is difficult to answer empirically for (at a minimum) two primary reasons:
- Endogeneity/Unobserved factors. For instance, personal, family, and neighborhood characteristics (e.g., family stability, access to health care, exposure to violence) may impact both mental health and the likelihood of food insecurity. Additionally, the direction of causality is unclear since mental health issues may lead to reduced likelihood of employment and thus food insecurity; conversely, food insecurity can increase stress and increase the likelihood of mental illness.
- Measurement error. Many studies of mental illness rely on surveys and self-reported measures of mental illness. This may lead to significant measurement error, particularly as stigma leads to misreporting of mental health.
How can we address these dual issues simultaneously? This is what a paper by Jansen et al. (2023) attempts to solve (see also presentation here). One clear solution would be to use instrumental variables, but finding a valid instrument is problematic since most factors correlated with mental illness are also directly correlated with food insecurity. Additionally, measurement error is more problematic when the key exposure variable (in this case the presence of mental illness) is binary.
The solution the authors use is to employ nonparametric partial identification methods developed in Kreider and Hill (2009) and Kreider et al. (2012). They apply these methods on data from the National Health Interview Survey (NHIS). They focus on patients who self-report “nonspecific psychological distress (NPD)” according to the Kessler (K-6) scale.
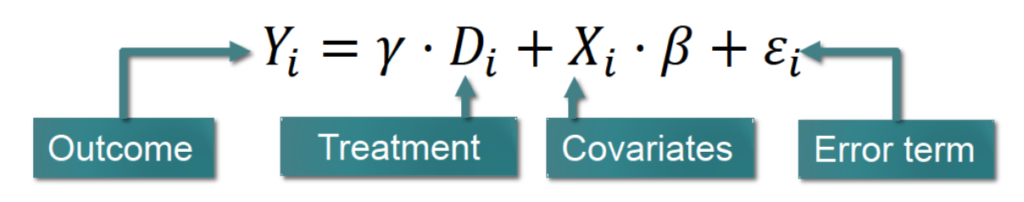
In the standard OLS regression model (see below), there may be endogeneity since the “treatment” (mental illness) may be correlated with the error term. Additionally, mental health status (D) is measured with uncertainty. For instance, let D* equal 1 if the individual is truly in mental distress and 0 otherwise. However, researchers only observe D, which is self-reported distress.
The key way the researchers solve this is by using the partial identification method. The goal is to estimate the following average treatment effect (ATE):
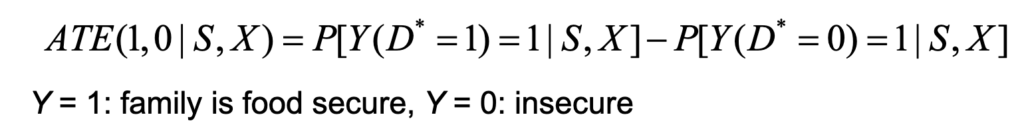
In this equation, Y(D* = 1) represents the potential food security outcome if adult were in distress; Y(D* = 0) represents the food security outcome if adult were not to be in distress.
Estimating this equation is problematic. To see why, let us decompose these values. Let us assume that P(Y=1|D*=1)=P(Y(1)=1|D*=1)*P(D*=1). If the true probability of mental distress–P(D*=1)–were known, this quantity could be estimated. However, the term P[Y(1)=1|D*=0], because it estimates a counterfactual not observed in the data (i.e., the level of food security that individuals without mental illness would have had if they did have mental illness).
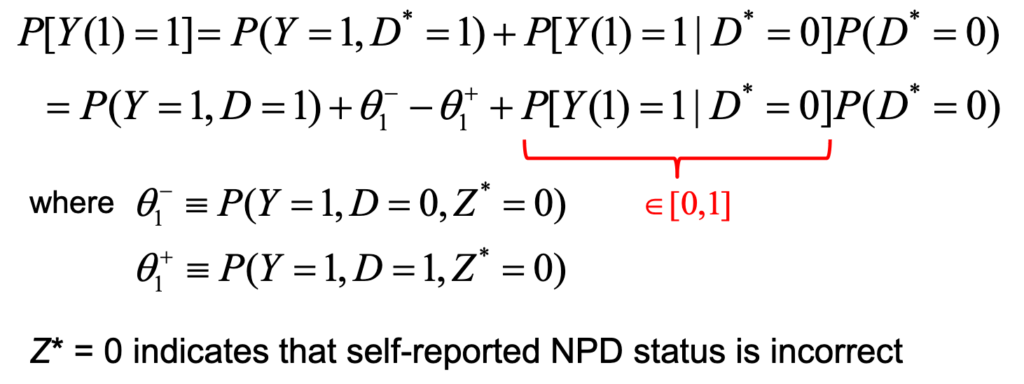
The second issue is that we don’t actually observe D*, so the first term is not estimable. The authors break down this term into something estimable [i.e., P(Y=1,D=1)] and measurement error terms. Because there is often sigma around mental illness, mental illness is likely to be under- rather than over-diagnosed. The authors claims that once can assume that there are no false positives so the θ1+=θ0+=0. The authors also assume the ratio of true vs. observed non-specific mental illness is proportionally the same as those reported for all types of mental illness. They use data reported from SAMHSA for this.
The also impose 3 different types of assumptions:
- Monotone treatment selection (MTS). This means that individuals who actually have mental illness are (weakly) less likely to have food security than those how actually do not have mental illness.
- Monotone instrumental variable (MIV). Here they assume that people living in areas with fewer food stores would have (weakly) less likely of being food secure.
- Monotone treatment response (MTR). Psychological distress would not improve food security on average.
Using these approaches, the author find that:
Applying relatively weak monotonicity assumptions on latent food security outcomes, we find that alleviating SMI would improve the food security rate by at least 9.5 percentage points, or 15%.
You can read the full paper here and there is a helpful summary slide deck (which I borrowed from extensively) here.


